Simple, Beautiful, and Predictable Class V Restorations
In general, people are retaining their teeth much longer than decades past. With this increase of tooth retention, the need to maintain and protect teeth has never been greater. Non-carious Class V lesions have become commonplace among an aging population. Toothbrush abrasion, acidic foods and drinks, and occlusal forces all contribute to the formation of non-carious Class V lesions. Class V lesions tend to be more prevalent in thin gingival biotypes.1 I see many untreated lesions enter my practice during new patient examinations. Often the patients report that their former dentist decided to watch or monitor those areas. I view these as missed opportunities to improve the function, longevity and beauty of our patient’s dentition. The decision to monitor, graft or protect these areas through bonding procedures is up to the individual dentist and patient. My clinical observations over 30 years of practice has led me to either recommend grafting procedures or bonding procedures to protect these vulnerable surfaces from further damage. This article will describe a simple and predictable technique to protect non-carious Class V lesions from further damage and help maintain the structural integrity of individual teeth and the overall dentition.
CLINICAL BACKGROUND
The patient presents with the complaint of pain to excessive temperatures on several teeth when eating. In particular she reports being very sensitive to cold food items on her maxillary left cuspid and first bicuspid. Clinical thermal testing confirms her report. Several treatment options were discussed including: a) desensitizing toothpaste, b) applying products designed to seal exposed dentin, c) grafting, and d) composite resin bonding. Ultimately, the patient decided that bonding was the most logical choice for her.
PRE-OPERATIVE CONDITION
Careful examination of the non-carious Class V lesions on the maxillary left cuspid and first bicuspid show loss of tooth structure apical to the CEJ of the tooth. This is likely caused by overly aggressive brushing and chemical wear from acidic foods and drinks. Occlusal wear from grinding is present and a likely co-contributor to this clinical condition. (FIG 1)

Non-carious Class V lesions on the maxillary left cuspid and first bicuspid show loss of tooth structure apical to the dentinenamel junction (DEJ) of the tooth.
Step 1: Selecting the Appropriate Shade
A test of several shades of Evanesce Flow are placed on the tooth and cured. If a more translucent result is desired, A1E Evanesce Flow (Clinician’s Choice) can be used. It has an opacity value of 80%, similar to natural enamel. If a more opaque material is desired A1U can be employed, as it is 85% opaque. In this case B1E and A1U were both tested. A1U is placed on the cuspid and B1E is on the bicuspid. A1U was selected as it has the best color match and opacity for this clinical case. This step must be done before any potential dehydration occurs. (FIG 2)

Before bonding, Evanesce Flow shades are tested. A1U is placed on the cuspid and B1E on the bicuspid. A1U was selected for best color match and opacity.
Step 2: Preparing the Soft Tissue
The teeth are anesthetized using buccal infiltration with 4% Septocaine, Epi. 1:100,000. Retraction cord is placed on the facial of each of the teeth to be restored. Ultrapak Cord (Ultradent) #000 is placed using a small non-serrated Slide Packer (Ultradent). Special care must be taken to prevent damage to the periodontium. Using the smallest cord that provides adequate retraction will help prevent damage to the attachment apparatus. (FIG 3)
Step 3: Preparing the Teeth
The teeth are prepared at the DEJ with an irregular bevel. This bevel varies in height and depth across the entire enamel portion of the DEJ. This irregular bevel accomplishes two things. First, it enhances the overall bond to tooth structure. Second, it is critical for hiding the restorative material and creating a seamless restoration. If a microetcher is available, the preparation should be abraded with 27 micron aluminum oxide. Sandblasting the surface of the tooth will remove contaminants and increase bond strength by creating microporosities on the surface of the tooth.
Step 4: The Adhesive Procedure
There are three choices for adhesive bonding in the cervical region of a tooth. A total-etch technique, a self-etch technique, or a selective-etch technique. To diminish staining potential and premature marginal breakdown, a selective etch technique is employed.2 This procedure is accomplished using Ultra-Etch, Peak SE and Peak Universal Bond (Ultradent). (FIG 4 and 5) Alternatively, a total-etch adhesive such as MPa Max (Clinician’s Choice) can we used. When total-etch adhesives are used, it is recommended to also use a glutaraldehyde-based desensitizer such as G5 (Clinician’s Choice).

Adhesive bond, Peak SE and Peak Universal Bond (Ultradent) is scrubbed into the prep using a microbrush.
Step 5: Restorative Material Placement
To make cervical restorations disappear seamlessly, the proper opacity of restorative material must be selected. In this case A1U Evanesce Flow (Clinician’s Choice) is used. This material possesses ideal thixotropic handling characteristics for easy placement and has an 85% opacity. Evanesce Flow has excellent optical properties resulting in an ideal blend with natural tooth structure. It is advised that the material be placed on the tooth and cured prior to beginning the procedure to ensure ideal color and opacity. The depth of the lesion should determine how many layers are required. In this clinical situation two layers are placed. (FIG 6)
Step 6: Contouring and Polishing the Restorations
To establish initial contour of the restoration a 12-fluted carbide finishing bur is employed. Care must be taken to maintain the height of contour in the cervical third of the tooth. This is accomplished with proper bur angulation. To do this, begin by refining the cervical third of the tooth first. The bur should only be cutting about 2mm from the tip. Once you have cleared the cervical area, the bur is flatted along the middle third of the tooth. Once the contouring is completed, the restoration is polished using A.S.A.P. All Surface Access Polishers, a two step polishing system from Clinician’s Choice. The design of these diamond-impregnated polishers very quickly establishes a high luster without damage to the established contours of the restoration. (FIG 7, 8 and 9)

Once proper contouring is complete, the purple A.S.A.P. Pre-polisher (Clinician’s Choice) is used to establish a quick polish.

The peach, A.S.A.P. Final High Shine Polisher (Clinician’s Choice) is used to establish a quick polish.
The Final Result
FIG 10 shows the final result. It is virtually impossible to see where the restoration ends and the tooth begins.
Successful Class V restorations require strict adherence to proper adhesive protocols, material opacity selection and finishing/polishing techniques. When restored properly, these composite restorations will service the patient for years to come. Drawing attention to the benefits of restoring these Class V with patients to help prevent future damage is not only efficacious but a good practice builder. This is accomplished by close adherence to the techniques described in the article.
REFERENCES
1. Cortellini, P., Bissada, N., Mucogingival conditions in the natural dentition: Narrative review, case definitions, and diagnostic considerations. J. Periodontol. 2018;89(Suppl 1):S204-S213
2. Peumans M. et al., Eight-year Clinical Evaluation of a 2-step, Self-etch Adhesive with and without Selective Etching. Dent Mater. 2010 Dec.

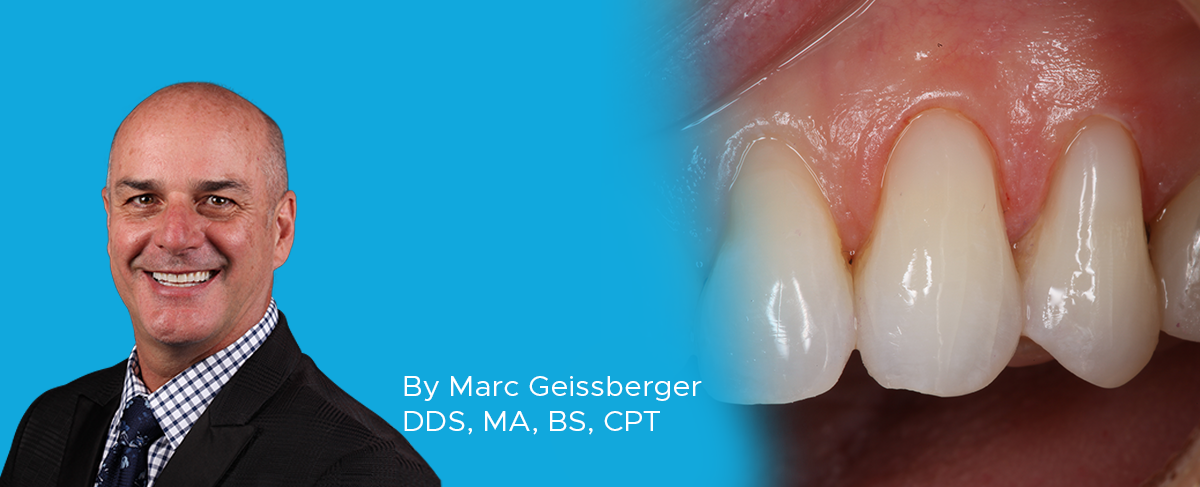
ABOUT THE AUTHOR
Dr. Geissberger graduated from University of the Pacific in 1991, obtaining his dental degree, and was elected to Omicron Kappa Upsilon as a student. Currently he is Adjunct Clinical Professor in the Department of Preventative and Restorative Dentistry at the University of the Pacific. He directed the University’s Aesthetic and Complex Care Clinic and teaches many hands-on CE courses in Restorative Dentistry. He maintains a private practice focused on reconstructive and esthetic dentistry in Greenbrae, CA.
Share This Article! Choose Your Platform
Related Articles
Using Affinity Crystal and Evanesce Flow in an Injection Molding Technique
By Susan Prater-Kudlats, DMD
The injection molding technique is gaining popularity for dental clinicians due to its wide array of procedural applications. This technique involves injecting a low viscosity resin composite through a transparent silicone index made from a diagnostic wax-up, aiming to replicate the mock-up.
Optimizing Aesthetics and Predictability in the Placement of Posterior Composite Resin Restorations
By Robert Lowe, DDS, FAGD, FICD, FADI, FACD
The term “universal” seems to be used frequently in the adhesion/composite resin materials world today. It has always been a struggle to find such a material that can adequately replace two very different types of tissues, namely enamel and dentin. Dentin is more opaque yet resilient, while enamel is
Simple Anterior Composite Restorations
By Nate Lawson, DMD, MA, PhD
A patient presented to the University of Alabama, School of Dentistry with fractured composites on the mesial incisal edges of his left central and lateral incisors that had been placed 20 years previously.
Restoring a Lateral Incisor to Proper Dimensions After Orthodontic Treatment
By Danièle Larose, DMD, AAACD
The most conservative method of restoring a Class IV fracture or correcting an anterior tooth size discrepancy is often composite resin.
Facially Driven, Single Opacity Composite Veneers
By Mark Bowes, BDS Rand
Tooth wear has become a common problem, and today it affects both young and old patients. Ceramic veneers have been the standard treatment for many years. However, patients today are looking for more conservative and more cost-effective ways to treat missing, diseased, and unsightly tooth structure.
Simplifying the Class II Composite with Bulk Fill: Efficiency Without Compromise – Clinical Article
By Marcos Vargas, BDB, DDS, MS & Kayla E. Erps, Senior Dental Student, University of Iowa
While restoring the posterior dentition, natural proximal contours, contact size, position and shape are integral to the function and longevity of both the restoration and remaining tooth structure. Composite dentistry has progressed to the point where restorations disappear into the surrounding tooth structure yet despite considerable improvements in both technique and materials, inconsistent results continue to be a challenge for many clinicians.