MPa Universal™ is a single-component, light-cure adhesive developed for use with self-etch, selective etch or total etch bonding techniques.
MPa Universal
Description
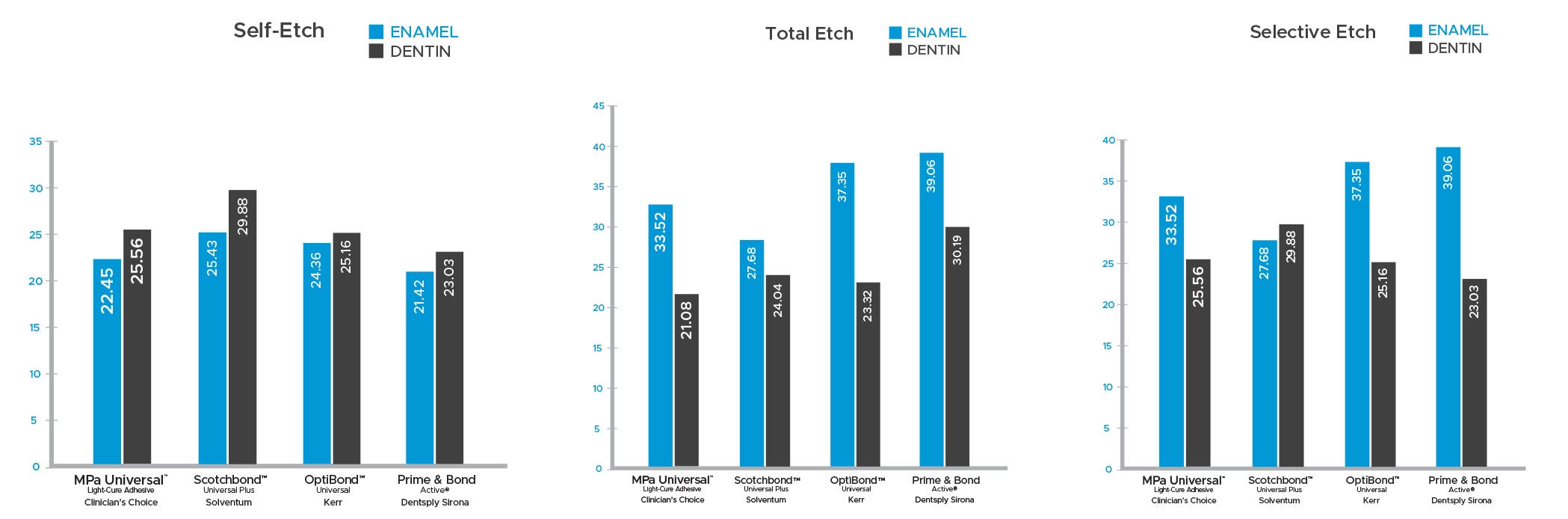
- Consistently High Bond Strengths: MPa Universal combines clinically proven chemistry of 10-MDP, HEMA, and ethanol as the solvent to generate high bond strength to dentin and enamel while providing a consistent dentin seal to reduce the chance of post-operative sensitivity.
- Low Film Thickness: The low film thickness of MPa Universal (< 10 microns) ensures ease of application without compromising the fit of indirect restorations.1
- Efficient & Affordable: MPa Universal combines excellent clinical results, easy application with precision dispensing, and is value priced in a bottle or unit-dose.
1For applications where light-cure cannot be ensured, use in combination with MPa Universal Dual-Cure Catalyst.
 Lawson, N. University of Alabama at Birmingham, School of Dentistry. Shear Bond Strength. September 2024.
Lawson, N. University of Alabama at Birmingham, School of Dentistry. Shear Bond Strength. September 2024.
Scotchbond™ is a trademark owned by Solventum Intellectual Properties Company. OptiBond™ is a trademark of Kerr Corporation. Prime & Bond Active® is a registered trademark of Dentsply Sirona, Inc.
Resources
Video
Instructions For Use / SDS
Click here to view the MPa Universal Light-Cure Adhesive Instructions for Use / SDS.
FAQ's
Following application, 20 seconds of agitation, and air-thinning (at least 5-10 seconds), light cure with a suitable halogen (quartz-tungsten-halogen) or LED (light-emitting diode) light unit.
You should always refer to the manufacturer’s instructions for use for the curing light you are using.
General curing guidelines are noted below.
| Curing Light Intensity(mW/cm2) | Recommended Curing time |
| <1000 | 20 seconds |
| ≥1000 | 10 seconds |
MPa Universal does not contain a silane and therefore is not indicated for lithium disilicate and other silicate ceramics that require a silane in the bond in order to achieve adhesion.
A “universal” adhesive is not a technical term but rather a clinical term. It implies that an adhesive can be used with or without phosphoric acid on dentin or enamel. In scientific writing, these adhesives are sometimes referred to as mild self-etch adhesives because they have a slightly less acidic pH (around 3) than typical self-etch materials (around 2). Another implication of a “universal” is the addition of monomers that allow bonding to indirect restorations, namely the monomers silane (for glass-based ceramics) or 10-MDP (for zirconia and some metals). Universal adhesives are typically single-bottle systems.
The use of a universal adhesive in a post and core technique would be no different from its use in any clinical scenario, except for the unique difficulty of light polymerization in the post space and the potential use of a dual- or self-cure material as the post cement and core material.
There are several methods to address the first clinical challenge of adequately curing the adhesive in the post space beyond aiming the light into the dark abyss of an often 6+ mm post space. First, a dual-cured adhesive may be used. These are typically 2-bottle systems, and they are not common. Second, the adhesive may be used with a dual-cured cement, which contains initiators to chemically-cure the adhesive, sometimes referred to as “contact cure.” Third, the adhesive may be co-cured with the post cement through a light-transmitting fiber post.
The issue with using a universal adhesive with a dual- or chemical-cured core material is that the acidity of universal adhesive can inhibit the amine-based chemical set of a core material. Therefore, some manufacturers recommend using a dual-cure activator with their universal adhesive if it will be used with any dual- or chemical-cured core material.
Two methods are commonly used in dental laboratories to determine the bond strength of an adhesive to tooth structure: the shear bond and the microtensile bond strength tests. In shear bond strength testing, the buccal or lingual surface of an extracted tooth is ground flat to dentin or enamel. After applying adhesive to that flat surface, a small button of composite (2.5 mm diameter) is bonded to the tooth using a plastic mold designed to ensure that the button is perpendicular to the flat section of the tooth. The force required to shear the composite button off of the tooth with a flat blade is recorded using a load cell. The shear bond strength of the adhesive is the maximum force required to dislodge the button divided by the surface area of the button. In the microtensile bond strength test, the occlusal surface of an extracted tooth is ground flat. After applying adhesive to that flat surface, a large increment of composite is placed over the entire flat surface of the tooth. The tooth is then sectioned axially into bars or “sticks (approximately 1 x 1 mm cross-section) – one side composed of tooth and the other composite. Either end of the bars is then attached to a fixture, which pulls the bars apart in tension and records the highest force before debonding. The debonding force divided by the cross-sectional area of the bars is used to calculate the microtensile bond strength.
Measuring bond strength can be performed after bonding to the tooth with a self-etch or etch-and-rinse technique. And both enamel and dentin may be tested depending on how deep the tooth is ground when preparing the flat surface for bonding.
The shear and microtensile bond strength tests mentioned previously have advantages and disadvantages. The microtensile bond strength testing is technically difficult to perform because sectioning the tooth/composite specimens into small sticks requires precise cutting, a process done with hand skill. There is debate about how to handle specimens which fail prematurely during handling – possibly excluding these premature failures will select only for the specimens within a group that have higher bond strength. Additionally, one tooth may provide multiple sticks, each providing a unique data point. Therefore, if a tooth with unfavorable bonding qualities (i.e., different mineralization) is included in a group, it may affect a large number of data points within that group. The disadvantage of the shear bond strength test is that when the load is applied to the composite button through a flat blade for debonding, the maximum stress on the interface is located at the area right where the blade is contacting the composite button. Therefore, any defects in the bond (i.e. a void) that are located at the area of the maximum stress may disproportionately affect the force required to debond the button. Therefore, the advantage of the microtensile bond test is that there is an even load applied across the surface area of the bond interface. The advantage of the shear bond strength test is that the test is less technically difficult, and therefore, premature failures do not occur. Additionally, each tooth has only one button bonded to it and therefore contributes to only one data point.
The most relevant test of adhesives is a split-mouth Class V retention study. The disadvantage of clinical trials, however, is that they are expensive and time-consuming, and differentiation between materials often does not occur until 5+ years of observation.
Regarding the relevance of immediate bond strength testing versus aged bond strength is important to consider. Bond strength may deteriorate due to stress on the bond (mechanical or thermal), hydrolytic degradation, or enzymatic degradation (MMPs). A common method to age a bond-strength specimen in the laboratory is thermo-cycling. In this test, specimens are cycled between 5-55C water baths. The thermocycling places stress at the bond interface due to the difference in coefficient of thermal expansion of the tooth and the overlying composite. An alternative method to age a specimen is to store it in water. Ultimately, the numerical bond strength of an adhesive is irrelevant; it is only relevant when compared to a reference. Therefore, the utility of immediate bond strength testing is often to compare new materials to existing materials with known clinical track records.
Enamel should be etched prior to use of any universal adhesive for several reasons. First, the pH of universal adhesives (around 3) is less acidic than previous self-etch primers (around 2) and phosphoric acid (less than 1). Second, universal adhesives do not provide a good etch pattern on enamel when observed under scanning electron microscopy. Finally, we performed a clinical trial with a common universal adhesive and reported that there was less marginal discoloration and less restoration debonding when enamel was etched.
When bonding to dentin, a self-etching technique can be used; however, it is important to agitate the adhesive, adequately evaporate all solvent from the adhesive, and adequately cure the adhesive. The optimal bonding technique is the selective etch method, in which enamel is etched with phosphoric acid and dentin is self-etched using a universal adhesive.
When dentin is etched with phosphoric acid, the mineral content of the dentin (hydroxyapatite) is removed, and demineralized collagen is left behind. To bond to dentin, an adhesive is applied, and it infiltrates into the demineralized collagen to form a hybrid layer. If dentin is over-etched, more mineral is removed, and the depth of demineralized collagen increases. Now, the mostly hydrophobic adhesive does not want to fully infiltrate the somewhat wet collagen. Therefore, there are voids at the bottom of the hybrid layer. These voids are more susceptible to hydrolytic or enzymatic degradation.
With some combinations of materials, using a self-etch adhesive will prevent the chemical set of a dual- or chemical-cure material overlying it. A clinical example would be using a self-etch universal adhesive on a prepared tooth that is light-cured and then covered by dual-cure core material that is allowed to chemically-cure. The incompatibility could cause a debond between the tooth and the core material. To prevent this situation, a dual-cure activator could be mixed with the universal adhesive before being applied to the tooth. Dual-cure activators contain salts (i.e., arylsulfinate salts), which when mixed with a self-etching adhesive, make the adhesive compatible with self- and dual-cure core materials or cements. A dual-cure activator does not make the adhesive itself capable of a chemical-cure.
A desensitizer is recommended for deep dentin. In deep dentin, the tubules are bigger/wider.
Even without usage of an etching gel, dentin resin tags can be observed with self-etch adhesives. Some of these tubules may be never sealed by the smear layers or opened by self-etch adhesives.
Product Configurations
- MPa Universal 5 mL Bottle (267001)
- MPa Universal Unit-Dose 50-pack (267000) Contains: 50 x 0.1 g unit-doses, 50 microbrushes
- MPa Universal Dual-Cure Catalyst 5 mL Bottle (267002)