The Missing Tooth: How the General Dentist and a Multidisciplinary Approach Can Achieve an Excellent Clinical Outcome
ABSTRACT
The successful replacement of a single anterior tooth involves a balance between esthetics, function, and anticipated longevity. In many cases, collaboration between the general dentist and one or more specialists is required to resolve the hard and soft tissue challenges that may arise in the process of achieving the desired outcome. This article describes how a collaborative approach between a cosmetic dentist and a specialist in replacing a single tooth produced the maximum benefit for the patient. Also discussed are how committing to a thorough examination and an educated patient improved the patient’s overall dental health and self-esteem.
INTRODUCTION
There are many options available today for patients presenting with a missing or failing tooth. While it can be a challenge to create a lifelike restoration that blends into the natural dentition, recontouring or augmenting the soft tissue can be very helpful in achieving natural esthetics. In addition to soft tissue esthetic procedures, correcting proportions with conservative orthodontic movements can greatly help patients through the unfortunate situation of anterior tooth loss.
CASE REPORT: PATIENT COMPLAINT AND HISTORY
A 30-year-old male presented with a chief complaint that several teeth were sensitive to cold. He also wanted information on how to correct the crowding of his lower teeth and whiten his smile. He had not been to a dentist for at least five years and thought he had never had a dental cleaning. The patient had experienced a traumatic dental injury many years earlier and had been treated with an endodontic post and crown on tooth #10. (FIG. 1-2)
CLINICAL FINDINGS AND DIAGNOSIS
A thorough hard and soft tissue examination was performed, including radiographs and clinical photographs. Periodontally, the patient presented with Class III calculus, several areas of recession, and a thin area of attached gingiva associated with the mandibular bicuspids and canines. In addition, periodontal bone loss was observed radiographically on the distal of tooth #18. A 6-mm clinical probing depth was noted in this area, likely due to an unerupted wisdom tooth. A 4-mm pocket with bone loss associated with #10 also was observed. A root fracture linked to a defective post and crown restoration on that tooth was suspected, as the pocket was clearly observed in one specific area. Several posterior interproximal carious lesions, including one of considerable size on #18, were identified, and treatment with composite restorations was recommended to the patient. An anatomical defect was present on the distal aspect of tooth #7. The patient had Class I occlusion with lower anterior crowding with working interferences present on teeth #4 and #5. The temporomandibular joints appeared healthy and asymptomatic. Apart from the dental issues, the patient was in excellent general health.
TREATMENT PLAN
The patient was advised that treatment of the existing carious lesions and periodontal issues should be completed prior to orthodontic correction of the anterior crowding. The extraction of #17 was critical to the restoration of #18; however, treatment of #18 was planned to be deferred until its periodontal condition improved. A deep cleaning was recommended to remove supragingival and subgingival calculus and ensure tissue health.
Orthodontics and implant placement: The risk of keeping the failing lateral incisor was discussed with the patient, as were options to replace it in the future. An endosseous implant, a Maryland bridge, and a removable partial denture were discussed as possibilities for the replacement of #10. Due to a size discrepancy resulting from the narrow widths of both lateral incisors, orthodontic treatment prior to the implant surgery would also create more ideal spacing for the implant in addition to correcting the crowding issues.1-4 The patient preferred a long-term and fixed solution and seemed to be more inclined toward the implant option after his orthodontic treatment.
Consultation with a periodontist was recommended regarding the possibility of utilizing an implant to replace #10 and to evaluate the bone loss associated with #18. Possible tissue changes after extraction were outlined, and it was suggested that a connective tissue augmentation graft, performed by the periodontist, might be preferable to achieve optimal esthetics regardless of whether the patient chose a bridge or implant.5
Home whitening and clear aligners: The treatment plan included the use of clear aligners with a pontic in the area of #10 in lieu of a temporary partial denture, until the implant was ready to be restored. It was suggested that the aligners could also be used to whiten the teeth with a home whitening kit. The patient was informed that following orthodontics, esthetic correction of the anatomical defect on #7 might be possible with the use of composite or a minimal-preparation porcelain veneer. The patient received a written list of the estimated costs of the different treatment possibilities. He wanted to take some time to consider the options and to seek financial assistance before starting treatment.
TREATMENT
Treatment commenced with the administration of local anesthesia, caries removal, and the placement of composite restorations on #2, #4, and #5, which had been diagnosed at the comprehensive exam.
The patient returned six months later with the post on #10 decemented. A root fracture was visible both clinically and radiographically. (FIG. 3) The prognosis was deemed poor and options for the replacement of this tooth were once again discussed.
The patient required more time to secure finances to proceed with the more permanent solution. He also wished to consult with the periodontist that we had recommended for implant placement. The post and crown were temporarily recemented and the patient was again given a written estimate of all treatment options. He was reminded that #18 required restoration due to caries, but declined treatment until after his periodontal consultation.
Orthodontics: The patient was scanned (iTero, Align Technology) and full photographic series (both orthodontic and AACD Accreditation) were obtained, followed by a thorough orthodontic examination. The latter revealed a Class I molar and canine occlusion, 20% overbite, and a 2-mm overjet. Lower anterior crowding was present, as were narrow arches and thinning attached gingiva in the areas of #22 and #27. The patient was informed that grafts might be necessary following orthodontic treatment, as well as the necessity of extracting #17 in order to restore #18 due to deep distal caries prior to starting orthodontic movements.
Three goals for orthodontic treatment were identified: correction of crowding, widening of both arches, and creation of equal spaces to enable #7 and #10 to be the same width. These orthodontic treatment objectives were planned using a 3D digital system that includes a Bolton analysis tool (ClinCheck, Align). Treatment time was estimated to be 10 months. The patient was given a consent form to take home for further review, as well as a prescription for a cephalometric radiograph.
After several months, the patient returned and received a referral to a maxillofacial surgeon concerning the extraction of #17. The possibility of endodontic treatment on #18 was also discussed due to the progression of caries. The patient proceeded with extraction of the semi-impacted wisdom tooth and, being eager to start orthodontic treatment, accepted accelerated orthodontics with a chairside accelerator (Propel Excellerator, Propel Orthodontics). Due to the quicker timeline, the ClinCheck was reviewed and modified, resulting in a treatment plan that included clear aligners (Invisalign, Align) plus retention in passive aligners.
Aligners and home whitening: After approximately one month of healing post-extraction, #18 was restored. At the same appointment, clear aligner attachments were placed with clear composite (Evanesce Enamel Clear, Clinician’s Choice). Soft tissue infiltration was performed employing four carpules of injectable anesthesia (3% Citanest Plain, Dentsply Sirona) followed by micro osteoperforations from distal of first bicuspids to distal of first bicuspids, upper and lower. A new Propel tip (using an implant driver at 45 RPM) was inserted to a depth of approximately 2mm into the cortical bone in all areas. At this point, the patient began the five month, five-day aligner change orthodontic movements (this is in contrast to the 14-day wear of each set of clear aligners usually prescribed). The patient also began a whitening regimen with 10% carbide peroxide gel (Opalescence, Ultradent) nightly for two weeks.
Implant placement: After consulting with the maxillofacial surgeon, the patient chose the implant option to replace #10. Extraction of #10 and immediate implant placement were planned during the final weeks of orthodontic treatment. This portion of treatment was timed to occur while the patient was in retention with aligner #23. Once the orthodontic movements were completed, limited occlusal equilibration was required as only the canines and one bicuspid needed an occlusal adjustment. A new scan was taken, and new custom trays were fabricated to be worn during orthodontic retention and the healing phase of the implant treatment.
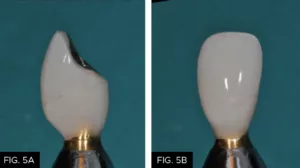
The periodontist extracted the failing #10, immediately placed a 4/3 x 15 mm endosseous implant (Biomet 3i), and performed a soft tissue augmentation procedure to achieve maximum gingival esthetics.6 With the healing cap in place, the clear aligners were fitted with a custom pontic to replace the extracted #10 for three to four months. Once the periodontist confirmed implant integration, impressions were taken to create a temporary crown on the implant. The surgeon then refined the soft tissue augmentation and the temporary crown was modified to ensure optimal esthetics (FIG. 4-5b).5,7
The healing time for the temporary crown was six months, during which time the patient was instructed to wear his aligners nightly. Once tissue healing was achieved (FIG. 6), the temporary crown was removed, and an implant transfer was placed and verified with a periapical radiograph. (FIG. 7)
A final impression was taken with polyvinyl siloxane impression material (Affinity, Clinician’s Choice). The final shade selection, multiple photographs for the technician, and a bite registration were also obtained at this time. (FIG. 8) The temporary crown was then re-cemented. An impression of the temporary crown was also sent to the laboratory to communicate the emergence profile to be replicated.
Final restoration: After consultation with the technician, the preferred definitive restoration was determined to be a custom zirconia implant abutment (FIG. 9) with a cemented crown (e.max, Ivoclar Vivadent). In consideration of the periodontist, it was decided to use temporary cement to ensure easier removal of the crown if it became necessary in the future.
Within a few weeks, the new abutment and crown were ready for a try-in. Shape and shade modifications were required, so the case was returned to the lab along with specific instructions and photographs. The temporary crown was once again recemented. Once the prescribed modifications were completed, a second try-in resulted in much-improved esthetics, to the satisfaction of both patient and doctor.
It was decided to place the abutment permanently and torque to 20 Ncm. Polytetrafluoroethylene tape was placed in the access cavity and composite (B1 Evanesce, Clinician’s Choice) was used to close the opening in the abutment. The crown was cemented (Temp-Bond, Kerr Dental). A radiograph was taken to ensure no subgingival cement was present. (FIG. 10)
(Note: in smile design, it is ideal that the two centrals be identical. On the other hand, it is normal and visually pleasing for the two laterals to be slightly different.) That said, the defect on #7 was now visually displeasing to the patient and he agreed to a slight shape modification using composite to better match #10. (FIG. 11)
No preparation was made; however, the biofilm was removed with a blaster (Bioclear). Tooth #12 was then etched and a single coat of adhesive (MPa Max, Clinician’s Choice) was applied. The tooth was restored employing a combination of nano-enhanced universal restorative composite (Universal, Evanesce, Clinician’s Choice), white opaquer and grey tint (Creative Color, Cosmedent), and a thin layer of Evanesce Enamel Clear (Clinician’s Choice). After light curing, the restoration was shaped and polished with a medium disc (Sof-Lex, 3M) and polishers (A.S.A.P., Clinician’s Choice). (FIG. 12)

Post-operative close-up retracted right lateral view (1:1) of #5-#9, showing corrected defect on #7 with the use of composite resin.
The patient was scanned for his final retention trays (Vivera, Align). After two weeks he returned for the tray insertion. He was instructed to wear his retainers nightly for at least two years, then two to three times a week.
FOLLOW-UP
The patient returned at two months and six months for overall assessment. The periodontist also saw him for a follow-up and was very happy with the results. Most importantly, the patient was pain-free and very pleased with the restorative outcome and overall treatment experience. (FIG. 13-15)
SUMMARY
Employing a multidisciplinary approach combining orthodontics, periodontal, and restorative solutions to help ensure complete harmony of the smile instead of focusing on a single tooth can offer our patients an optimal esthetic outcome. This is true not only for the missing tooth challenge but in restorative cases as well. The use of clear aligners has improved the esthetics and longevity of the author’s patients’ restorations. Adding orthodontics in the general dental practice is an excellent asset to
enhance patient outcomes.
ACKNOWLEDGMENT
The author thanks periodontist Dr. Alexandre Taché (Pointe-Clair, QC, Canada), for his clinical work with the case discussed in this article; and Mark Willes, CDT (Experience Dental Studio; Lindon, UT), for his assistance and skill with the case.
REFERENCES
-
Martegani P, Silvestri M, Mascarello F, Scipioni T, Ghezzi C, Rota C, Cattaneo V. Morphometric study of the inter proximal unit in the aesthetic region to correlate anatomic variables affecting the aspect of soft tissue embrasure space. J Periodontol. 2007 Dec;78(12):2260-5.
-
Carnio J, Carnio AT. Papilla reconstruction: interdisciplinary consideration for clinical success. J Esthet Restor Dent. 2018 Nov;30(6):484-91.
-
Bello A, Jarvis RH. A review of aesthetic alternatives for the restoration of anterior teeth. J Prosthet Dent. 1997 Nov;78(5):437-40.
-
Pini NP, de-Marchi LM, Gribel BF, Ubaldini ALM, Pascotto RC. Analysis of the golden proportion and width/height ratios of maxillary anterior dentition in patients with lateral incisor agenesis. J Esthet Restor Dent. 2012 Dec;24(6):402-14.
-
Pini NP, de-Marchi LM, Gribel BF, Pascotto RC. Digital analysis of anterior dental aesthetic parameters in patients with bilateral maxillary lateral incisor agenesis. J Esthet Restor Dent. 2013 Jun;25(3):189-200.
-
Yu SH, Tseng SC, Wang HL. Classification of soft tissue grafting materials based on biologic principles. Int J Periodontics Restorative Dent. 2018 Nov/Dec;38(6):849-54.
-
Eghbali A, Seyssens L, de Bruykere T, Younes F, Cleymaet R, Cosyn J. A 5-year prospective study on the clinical and aesthetic outcomes of alveolar ridge preservation and connective tissue graft at the buccal aspect of single implants. J Clin Periodontol. 2018 Dec;45(12):1475-84.

ABOUT THE AUTHOR
Dr. Danièle Larose’s private practice, in St-Laurent, Québec, Canada, focuses on conservative cosmetic and reconstructive dentistry. Years of daily practice have enabled her to develop her “how did you do that? — instant orthodontics” and “smile lift” techniques. Dr. Larose graduated from the University of Montreal in 1997. She attended the Dawson Institute and the Las Vegas Institute for Advanced Dental Training. For the past several years she has been receiving great reviews teaching full-day hands-on classes in Canada and the U.S. devoted to anterior aesthetic techniques. She is a member of the LVI Study Club, Implantology Study Club, AACD, CAED, Invisalign Study Club, and Ordre des dentistes du Québec.
Share This Article! Choose Your Platform
Products Mentioned in this article
Related Articles
Take 5: 5 Restorative Clinicians’ Take on A.S.A.P. All Surface Access Polishers
5 Restorative Clinicians' Take On A.S.A.P. All Surface Access Polishers.
Take 5: 5 Restorative Clinicians’ Take On Evanesce Nano-Enhanced Universal Restorative
5 Restorative Clinicians' Take On Evanesce Nano-Enhanced Universal Restorative.
A Conservative Approach to Restoring the Worn Anterior Dentition
By Newton Fahl, DDS, MS
Long-term restorative treatment of the worn dentition can be a complex endeavour and possibly extend beyond the scope and experience of the general dentist. Additionally, restoration of this compromised dentition may require other health disciplines’ involvement to address any psycho-social factors that may limit the long-term success of the restorative treatment.