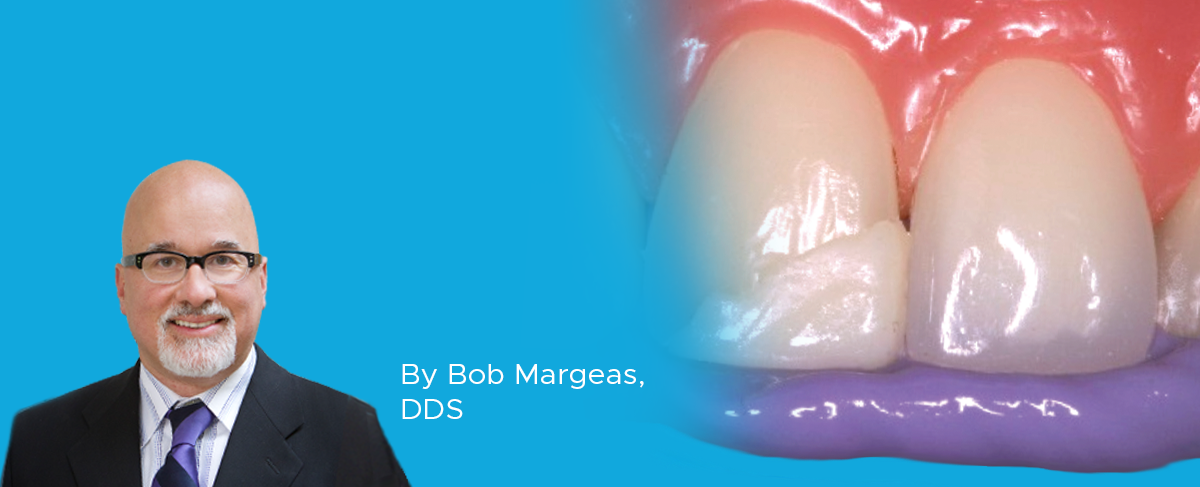
The Lingual Matrix Technique
By Bob Margeas, DDS
From the one-shade to the more complex Class IV requiring layering of opacities, the simple fabrication of a lingual matrix can greatly simplify your technique while minimizing finishing time. The lingual matrix establishes optimal incisal length and lingual contour, enabling more accurate placement of subsequent layers. This accuracy translates into procedural efficiency and a more predictable restorative outcome.
Using the existing restoration, or, if necessary, mock-up a restoration using some unwanted or seldom-used composite, keeping in mind that only the incisal edge and lingual contour and contacts need to be accurately established. Once the mock-up is cured, apply a thick layer of Template™ Matrix Material (Clinician’s Choice®) to the lingual of all six anterior teeth, ensuring that the material doesn’t extend beyond the facio-incisal line angle (Step 1).

a line corresponding to the fracture is scribed onto its inner surface. A very thin, uniform layer of Evanesce™ Enamel FX White composite is placed up to the scribed line (Step 2). The matrix is placed back onto the teeth and this lingual layer is attached to the etched and bonded tooth and light cured (Step 3). Controlled placement of subsequent layers of Evanesce can now be carried out without the lingual matrix in place (Step 4).
This fast and simple step of creating a lingual matrix with Template Matrix Material makes the complicated layered placement of a Class IV composite easier, more predictable and efficient (Step 5).
Join the Hands-OnLine LIVE™ course, Mastering the Class IV Restoration, and complete this technique under the live direction of Dr. Bob Margeas. See handsonlinelive.com or next page for course schedule and to register.

ABOUT THE AUTHOR
Dr. Margeas graduated from the University of Iowa College of Dentistry in 1986 and completed his AEGD residency the following year. He is currently an adjunct professor in the department of Operative Dentistry at the University of Iowa. He is Board Certified by the American Board of Operative Dentistry. He is a Diplomate of the American Board of Aesthetic Dentistry, a Fellow of the Academy of General Dentistry, American Society for Dental Aesthetics and International Team of Oral Implantologists (ITI). He has written numerous articles on esthetic and implant dentistry, and lectures and presents hands-on courses nationally and internationally on those subjects.
Products Mentioned in this article
Related Articles
Ultimate Esthetics Using Non-VITA Shades for Diastema Closure
By Marcos Vargas, BDB, DDS, MS
Spaces between anterior teeth are a common occurrence, and for some, this can be an unattractive feature that they may be looking to correct, especially spaces in the midline.
The Starburst Bevel: A Simple Solution for Enhanced Esthetics and Retention
By Susan McMahon, DDS, AAACD, FAGD
Developing a protocol for your Class IV technique is essential for attaining predictable and long-lasting esthetic restorations. Depending on the size of the Class IV and the presence of incisal translucency and surface characteristics of the adjacent teeth, for instance, your anterior composite protocol should also be both flexible and versatile.
Take 5: 5 Restorative Clinicians’ Take On Evanesce Nano-Enhanced Universal Restorative
5 Restorative Clinicians' Take On Evanesce Nano-Enhanced Universal Restorative.
Multilayer Composite Technique for Extraordinary Outcomes in Common Clinical Situations
By Megan Shelton, DMD
Responsible esthetic dentistry embraces the notion of optimizing esthetic results with minimal tooth structure removal while acknowledging the inherent risk to the dentition as a result of any restorative intervention. It is this systemic approach that underlies my esthetic treatment planning and, more often than not, multilayered composite allows me to provide the highest quality esthetic dentistry with the least impact to tooth structure.